UNDERSTANDING DISCOGENIC & FACETOGENIC PAIN
What is Discogenic Pain?
Discogenic is pain originating from a damaged vertebral disc, particularly due to degenerative disc disease. About 40% of all chronic spine pain is related to a problem in one or more intervertebral discs.
Causes of Discogenic Pain:
- Disc degeneration
- Prior injury or accident
- Osteoarthritis
- Minor instability
- Prior low back surgery
- Mechanical low back pain

Common Symptoms of Discogenic Pain:
- Achy pain in your back that may refer to the leg
- Pain usually worsens when the spine is compressed
- Typically, discogenic pain is associated with activities that increase the pressure within the intervertebral disc (intradiscal pressure)
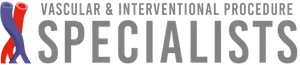
What is Facetogenic Pain?
Facetogenic is pain originating from the facet joint. The affected individual will find it difficult to bend twist, or rotate to the sides because of pain.
Causes of Facetogenic Pain:
- Repetitive stress and/or cumulative low-level trauma
- Prior injury or accident
- Osteoarthritis
- Minor instability
- Prior low back surgery
Common Symptoms of Facetogenic Pain:
- Axial low back pain with referred pain perceived in the flank, hip, and thigh
- Difficulty bending, twisting, or rotating to the sides
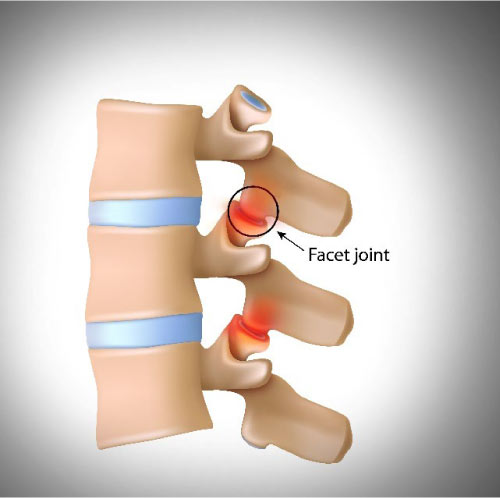
What is Spinal Stenosis?
Spinal stenosis is a narrowing of the spaces within your spine, which can put pressure on the nerves that travel through the spine. Spinal stenosis occurs most often in the lower back and the neck.
Causes of Spinal Stenosis:
- Repetitive stress and/or cumulative low-level trauma
- Prior injury or accident
- Osteoarthritis
Common Symptoms of Spinal Stenosis:
- Numbness or tingling in foot, leg, arm or hand
- Weakness in foot, leg, arm or hand
- Problems with walking and balance
- Pain or cramping in one or both legs when you stand for long periods of time or when you walk, which usually eases when you bend forward or sit
- Back or neck pain
- Pain on extension
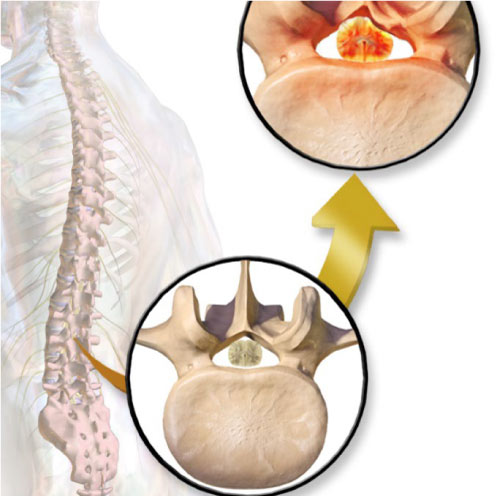
THE ION FACET SCREW SYSTEM & 3D GRAFTRASP SYSTEM
Two Systems Used in Combination:
The Ion Facet Screw System and 3D GraftRasp System are two standalone systems that are often used on the same patient.
The Ion Facet Screw System:
The Ion Facet Screw System has been designed to achieve optimal stabilization and fusion potential through a minimally invasive approach. The unique instrumentation set properly prepares bilateral facet joints for the implantation of the titanium Ion Facet Implant.
Advantages:
- Cleared from FDA as standalone device without the need for other fixation supplements
- Minimally disruptive technique can reduce operative time, tissue trauma, blood loss, and post-operative pain relative to more invasive fusion devices.
- Minimal steps for joint preparation and implantation.
- Provides stabilization to the posterior spinal column.
- Nanotex® surface technology developed with osteointegration in mind
*See Ion Facet Screw System Surgical Technique for Indications, contraindications, cautions, and warnings
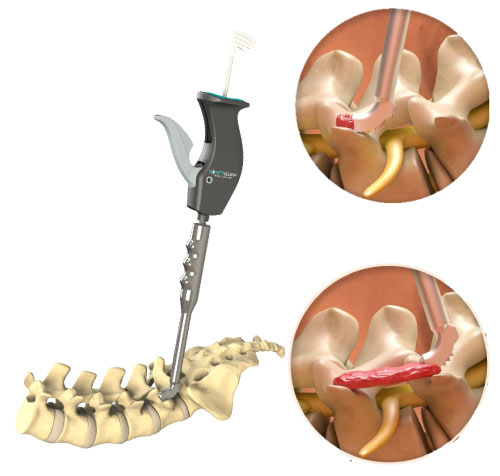
The 3D GraftRasp System:
Only FDA-cleared system on the market for decortication and bone graft delivery to an orthopedic site. It is often used for posterolateral fusions to decorticate the transverse process and/or facets of two adjacent levels and then to deliver bone graft across the bleeding bone. Removal of the cortical bone layer exposes the cancellous layer which contains the growth factors, cells, and vascular supply necessary to achieve a fusion.
Advantages:
- Decortication of the transverse process/facet joint and delivery of bone graft to those locations in a minimally invasive technique
- No hardware necessary for fusion
- Can be used in the destruction of the medial branch of the spinal nerve root that innervates the facet joint.
*See 3D GraftRasp System Surgical Technique for Indications, contraindications, cautions, and warnings.
Provider Treatment Process
Facet Joint Pain Treatment Options:
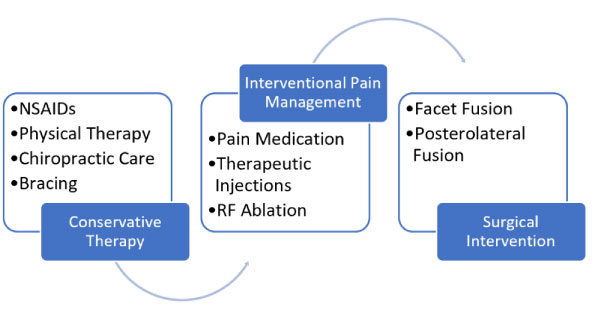
Evaluation & Therapy Considerations
Potential Indications:
- Facet Mediated Pain
- Stabilization of the lumbar spine with decompressive procedures where minor instability exists
- Lumbar DDD
- Minor instability
- Adjacent level disease
- Mild foraminal stenosis
- Mild canal stenosis
- Posterior supplemental fixation to interbody fusion (ALIF, LLIF, TLIF, PLIF, OLIF)
- Adjunct to interspinous device
When it is suspected that your patient’s symptoms could be attributed to the indication listed above, it is recommended to begin with conservative treatment options such as physical therapy.
Interventional pain management therapies, including pain medications or therapeutic injections, are often the next step. These therapies may provide some patients temporary relief, but often only work short term. Radio-frequency ablation (RFA) has also been used with some success, but similar to injections, may only provide temporary relief.
Posterolateral fusion should be considered after non-surgical interventions have failed to provide a patient with an enduring solution to their pain. Fusing adjacent vertebrae in the spine, thereby eliminating pain-generating instability, can provide enduring pain relief.
What To Expect – Patient Guidelines
The suggestions below are provided as guidance only and should be tailored specifically to each patient. Patients should follow all instructions and recovery guidelines as directed by their physician.
Pre-Procedure
- Discuss all medications you are taking before your surgery and if you will need to
make any changes up to your procedure date (i.e. NSAIDS, blood thinners,
supplements). - Arrange for a reliable friend or relative, over the age of 18, to drive you home after your procedure and stay with you for the first 24 hours after surgery.
- No smoking before and after the procedure according to physician’s instruction
Day of Procedure
- Wear comfortable, loose clothing and flat shoes; remove all jewelry
- Anesthesia will be provided during the procedure—general anesthesia or local sedation will be used depending on your physician’s discretion
- A staff member will take you into the operating room and monitors will be attached
to measure your pulse, oxygen level, and blood pressure - After your procedure, you will be moved to the recovery area and will be able to be
ambulatory once you clear anesthesia
Post-Operative Expectations
- Avoid showering for 3 days after surgery. After confirming with the doctor on your post-op appointment. Let the water flow over the incision area, do not aggressively scrub.
- Avoid baths, hot tubs, spas, or swimming in the pool or at the beach for 2 weeks.
- Avoid exaggerated bending/twisting or lifting/pushing 15 pounds or more for up to 6 weeks.
- Avoid NSAIDs to ensure the desired inflammatory response
Other Considerations
- Walk on flat and non-slippery surfaces as much as you feel comfortable. (follow physician instructions on assistance devices)
- Maintain your regular diet
- Take pain medications as prescribed by your physician
- No driving within 72 hours while taking narcotic medications or anesthesia.
- No exercise program is allowed until you are released by your physician to do so.